CVS / Pharmacy Rebate – A CVS/pharmacy rebate is a fantastic strategy to reduce the cost of medical treatment. But you need to think about what you’re committing to.
Co-pay discounts drive up medical expenses.
Prescription medicine costs are rising despite some patient assistance programs and copay savings. In comparison to 2010, the median amount that patients pay for medications has increased by 53%. The profitable information is that there exist methods for lowering prescription drug costs.
Utilizing rebates is one technique to reduce the price of prescription drugs. Pharmaceutical stores and health insurance companies receive discounts from manufacturers. These rebates might not, however, directly impact patients’ out-of-pocket expenses.
CVS Health Corp. is one of the biggest pharmacy benefit administrators. Recently, this business unveiled a pharmaceutical benefit option that ensures 100% of rebates. The new initiative aims to increase drug cost predictability.
Typically, a pharmacy benefit manager (PBM) bargains with a drug manufacturer to obtain a discount for the medication. The PBM then distributes the savings to patients and insurance companies. The AWP-based pharmacy benefit payments are the most typical.
According to experts from the University of Southern California, 9.5 million prescriptions were completed during the first half of 2013. A generic heart medicine costs only $35 during this time instead of the customary $800 to $1,200.
The pharmacists at CVS decline to fill prescriptions for common medications.
CVS pharmacists have been charged with acting in a way that could have had detrimental effects on clients in the future during the national drug epidemic. The company’s action might intensify discussions over the drug problem.
The business and the Drug Enforcement Administration have a three-year compliance agreement. The business also unveiled a set of prescription guidelines last year that might aid in the fight against the epidemic of addiction. In reaction to a Supreme Court decision, certain rules were created.
The business is also installing 750 drug disposal kiosks inside its retail locations. Customers will be able to get rid of unneeded drugs and controlled substances at these kiosks.
The business recently disclosed plans to restrict the dosages of opioid painkillers for new patients. In February, these regulations will become effective.
Guidelines for the appropriate prescription of opioids have also been developed by the CDC. Though some pharmacies continue to refuse to fill prescriptions, the majority of healthcare organizations have made the CDC’s recommendations part of their policies.
Some of the most typical opioid addictions begin with a painkiller prescription. Pharmacists are not allowed to refuse to fill a prescription for medical reasons under the legislation of some states.
Beginning in 2019, customers of CVS Caremark can adopt the guaranteed net cost model.
In a recent briefing, CVS Caremark revealed that starting in 2019, customers would be able to choose a new pricing model called “Guaranteed Net Cost.” Based on plan use, average wholesale price inflation, and anticipated changes in the drug mix, this new model will determine net costs.
The corporation will also streamline the financial arrangements supporting PBM contracts with the new approach. In addition, choosing a PBM based on the net cost per claim will be simpler for plan sponsors.
Additionally, assisting PBM clients in managing outside vendors is the new strategy. To address this, CVS Health is creating an intelligent engagement platform that will connect the customer journey, personalize content management, and establish situational context.
The new model also gives plan sponsors the option to decide whether to pass rebates on to patients. For instance, Aetna covers members’ out-of-pocket expenses when they go to a qualified telehealth provider. Members can also keep track of their mood, location, and benefit information with the aid of the Aetna Mobile app.
The function of CVS as a go-between for pharmaceutical firms and customersThe public is highly concerned about the possibility that CVS acts as a middleman between drug manufacturers and consumers. The issue is how properly the firm manages reimbursements to neighborhood pharmacies.
The FTC recently declared that it would investigate the industry of prescription drug middlemen. It is looking into how patients’ access to reasonably priced prescription pharmaceuticals is impacted by vertically integrated PBMs.
PBMs, often known as pharmacy benefit managers, serve as a liaison between prescription drug producers and insurance. They work out discounts with pharmaceutical companies and pay pharmacies for distributing prescriptions. In addition, they can raise prices by implementing profit-maximizing measures. Prescription medications become more expensive as a result, and necessary therapy is delayed.
The CMS reported in 2016 that 10% of all healthcare costs were spent on prescription drugs. Costs were sometimes rising by double digits. The FTC has asked for a study to look into the procedures of six significant PBMs.
One of the biggest pharmacy benefit management companies in the country is CVS. It manages about 10,000 pharmacies, including walk-in clinics and specialty pharmacies. The PBM division generates around 60% of its total income.
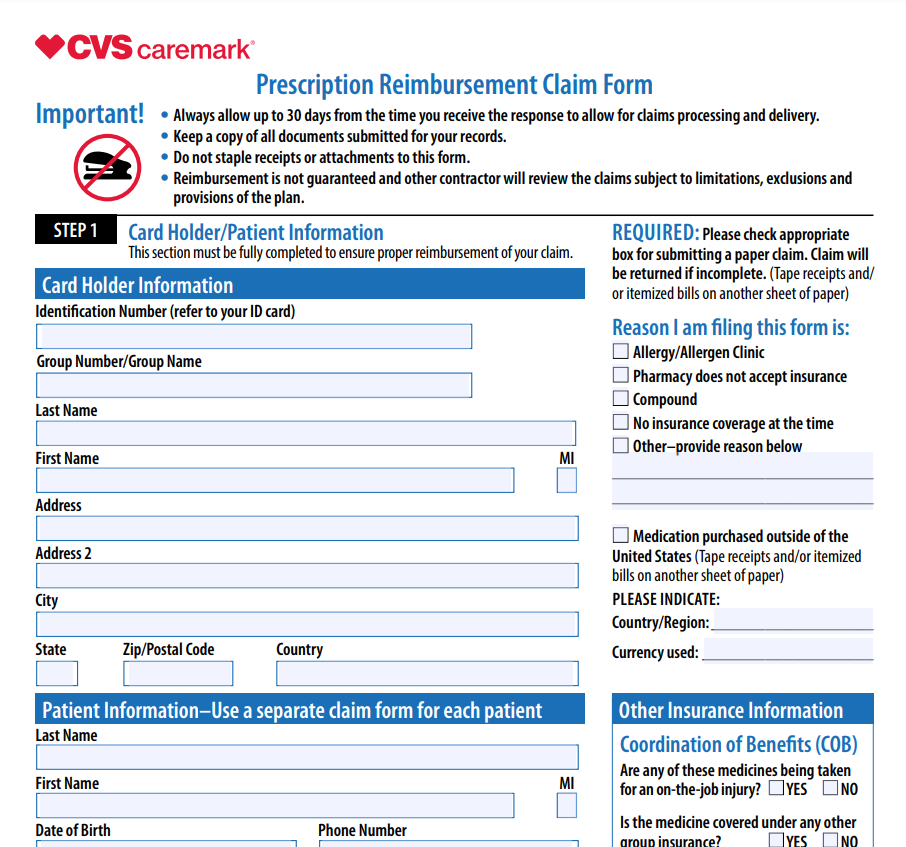
Download CVS / Pharmacy Rebate Form 2024