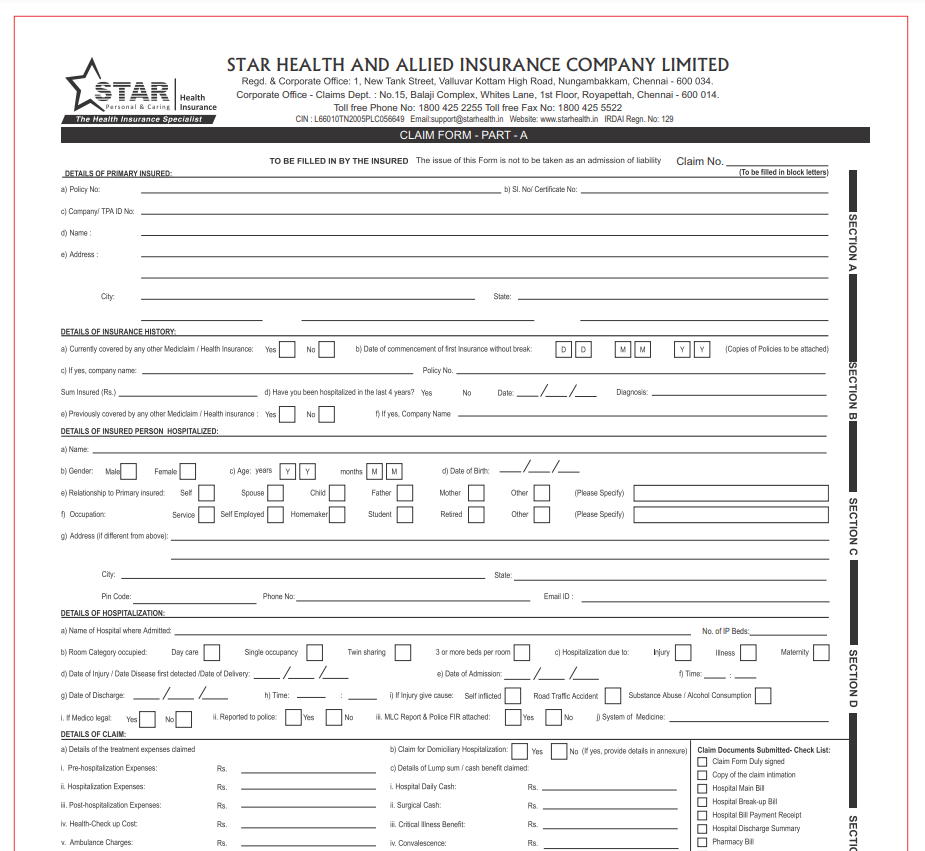
Reimbursement Form Star Health – If you’re a member of Star Health Insurance, you can get your claim form by going to the office of your insurance company or by going to the Star Health Insurance website. The form is also available at the insurance counter in a hospital. Normally, this form includes details about you as an insured patient, the benefit you’re looking for, and your insurance information. Instructions for other forms that you must submit with the claim could also be included. The provider can assist you in filling out the appropriate forms if you’re confused which ones to submit.
Form of Pre-Authorization
Before being admitted, you should submit a Star Health Pre-Authorization form if you’re thinking about staying in the hospital. You can use this form to help you submit your claim and to assist your insurer in reviewing your case. Following treatment, the insurer will get in touch with you to get more information, and you will then go through the claim reimbursement process.
The pre-authorization form may be printed from the insurer’s website or completed online. A copy of your policy or identification cards should be included with the fully completed form. Typically, your insurer will cover a portion of your anticipated costs, and you will be responsible for the balance when you leave the hospital. However, you need to be aware that unforeseen costs won’t be covered.
The form should be self-explanatory and contain all necessary details concerning the surgery you will be undergoing. Include the nature of your condition and the medical care you received. You must also include any receipts or medical invoices related to the operation. Finally, confirm that your policy is in effect and that you timely renewed it.
medical expenses
It’s crucial to present the actual medical bills together with a copy of the claim form when submitting a claim. The insurance provider will be able to assess if the benefit you are requesting is covered if you have the original bills. If not, you could have to pay out of pocket for the service.
You can be entitled to financial compensation from Star Health if you receive care outside of the network. You must deliver the needed supporting documentation to your Star Health insurance office in order to be qualified for payment. This evidence may be in the form of medical records or other proof indicating you had care at the same institution. The entire amount of the final bill won’t be paid until all insurance payments are in.
You may be qualified for payment for daycare procedures if you have a Star health insurance coverage. Other insurance plans often do not cover these operations. Additionally, you can be eligible for payment for procedures carried out by complementary therapies like ayurveda or homoeopathy.
No-cash claim
The insured must complete the claim form and provide all required documentation in order to begin a claim for medical expenditures with Star Health. You can get the refund claim form from the insurer’s website or customer service. A reimbursement claim can be processed through the insurer’s network hospitals, but a cashless claim needs a pre-authorization letter to get started.
You should submit a cashless claim with Star Health for your medical expenditures if you are injured or ill. When you submit this straightforward and uncomplicated form, the insurer will pay back your costs. Using the form is an easy and quick approach to acquire the cash you want for immediate medical attention. There is a significant probability that you will be able to receive the money you require without having to worry about it because millions of hospitals in India accept this kind.
After completing your cashless claim form, send it to Star Health online. Your claim will be delivered to you in as little as two hours. The insurer will get in touch with the hospital to confirm the specifics of your claim after reviewing the information.
documentation validation
The Star Health reimbursement form’s document verification section is crucial to the claims procedure. This will provide you the chance to confirm that the medical care was given by the appropriate provider. For instance, if the records reveal that you did not obtain medical care from a hospital that was not linked with Star Health, you can be confident that your claim would be rejected.
Your original medical bills and any pertinent test results must be submitted if you need to make a claim for reimbursement from Star Health. Usually, you’ll need to give both extra copies and the original bills. You will be able to determine whether the benefit you are requesting is covered under your plan by providing the original bills. You will have to pay out of pocket if it is not.
Within 15 days of receiving care, you must submit a claim for payment through the Star Health reimbursement system. You have two options for filing your claim: online or by mail. The business will then provide you a claim reference number and get in touch with you to request the required paperwork.
Download Reimbursement Form Star Health 2025